| Alcoholism | |

| |
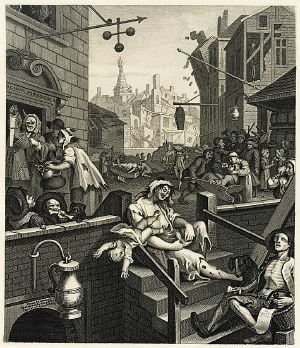
| "King Alcohol and His Prime Minister" c. 1820 | |
| Symptoms | Drinking large amounts of alcohol over a long period, difficulty cutting down, acquiring and drinking alcohol taking up a lot of time, usage resulting in problems, withdrawal occurring when stopping |
|---|---|
| Complications | Mental illness, delirium, Wernicke–Korsakoff syndrome, irregular heartbeat, cirrhosis of the liver, cancer, fetal alcohol spectrum disorder, suicide |
| Duration | Long term |
| Causes | Environmental and genetic factors |
| Risk factors | Stress, anxiety, inexpensive, easy access |
| Diagnostic method | Questionnaires, blood tests |
| Treatment | Alcohol detoxification typically with benzodiazepines, counselling, acamprosate, disulfiram, naltrexone |
Alcoholism, also known as alcohol use disorder (AUD), is, broadly, any drinking of alcohol that results in mental or physical health problems. Medically, alcoholism is considered both a physical and mental illness. Symptoms of alcoholism include drinking large amounts of alcohol over a long time period, having difficulty reducing alcohol consumption, spending large amounts of time acquiring and drinking alcohol, alcohol usage results failing to fulfill responsibilities, social problems, health problems, and risky behavior, withdrawal occurs when stopping, and the person has developed alcohol tolerance.
Both environmental and genetic factors are associated with alcoholism, and alcohol's inexpensive cost and easy accessibility increase the risk. Attitudes and social stereotypes create barriers to the detection and treatment of alcohol abuse and fear of stigmatization leads people to avoid admitting they have a dependency on alcohol. The multiplicity of reasons that lead to alcohol abuse require a combination of approaches, both physical and psychological, for successful treatment. The various health problems associated with long-term alcohol consumption are generally perceived as detrimental to society, both in financial costs due to lost labor-hours and cost of treatment, and in social costs in terms of disruption of family and other relationships. Addressing the problem of alcohol abuse is thus of great value both to the individuals involved and to society in general.
Definition
The Joint Committee of the National Council on Alcoholism and Drug Dependence and the American Society of Addiction Medicine produced the following definition of alcoholism:
a primary, chronic disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. The disease is often progressive and fatal. It is characterized by impaired control over drinking, preoccupation with the drug alcohol, use of alcohol despite adverse consequences, and distortions in thinking, most notably denial. Each of these symptoms may be continuous or periodic.[1]
History
The name "dipsomania" was coined by German physician C.W. Hufeland in 1819 to describe a medical condition involving an uncontrollable craving for alcohol.[2][3] The term "Dipsomania" is still used to describe a particular condition of periodic, compulsive bouts of alcohol intake.[4] The term "alcoholism" was first used in 1849 by the Swedish physician Magnus Huss to describe the systematic adverse effects of alcohol.[5]
Alcohol has a long history of use and misuse throughout recorded history. Biblical, Egyptian, and Babylonian sources record the history of abuse and dependence on alcohol. In some ancient cultures alcohol was worshiped and in others, its abuse was condemned. Excessive alcohol misuse and drunkenness were recognized as causing social problems even thousands of years ago. However, the defining of habitual drunkenness, as it was then known, and its adverse consequences were not well established medically until the eighteenth century. In 1647 a Greek monk named Agapios was the first to document that chronic alcohol misuse was associated with toxicity to the nervous system and body which resulted in a range of medical disorders such as seizures, paralysis, and internal bleeding. In 1920 the effects of alcohol abuse and chronic drunkenness boosted membership of the temperance movement and led to the Prohibition on alcohol (United States), a nationwide constitutional ban on the production, importation, transportation, and sale of alcoholic beverages that remained in place until 1933. This policy resulted in the decline of death rates from cirrhosis and alcoholism.[6]
Diagnosis
Alcoholism, also known as alcohol use disorder (AUD), is, broadly, any drinking of alcohol that results in mental or physical health problems.[7] The disorder was previously divided into two types: alcohol abuse and alcohol dependence.[8]
In a medical context, alcoholism is said to exist when two or more of the following conditions are present: a person drinks large amounts of alcohol over a long time period, has difficulty cutting down, acquiring and drinking alcohol takes up a great deal of time, alcohol is strongly desired, usage results in not fulfilling responsibilities, usage results in social problems, usage results in health problems, usage results in risky situations, withdrawal occurs when stopping, and alcohol tolerance has occurred with use.
Description
The term "alcoholism" is commonly used by laypeople, but the word is poorly defined. The World Health Organization (WHO) calls alcoholism "a term of long-standing use and variable meaning," and use of the term was disfavored by a 1979 WHO expert committee. The Big Book from Alcoholics Anonymous (AA) states that once a person is an alcoholic, they are always an alcoholic (but others note that many do recover), but does not define what is meant by the term "alcoholic" in this context.[9] In 1960, Bill Wilson, co-founder of Alcoholics Anonymous (AA), said:
We have never called alcoholism a disease because, technically speaking, it is not a disease entity. For example, there is no such thing as heart disease. Instead there are many separate heart ailments, or combinations of them. It is something like that with alcoholism. We did not wish to get in wrong with the medical profession by pronouncing alcoholism a disease entity. We always called it an illness, or a malady – a far safer term for us to use.[10]
AA describes alcoholism as an illness that involves a physical component and a mental obsession, such that "Alcoholics suffer from a (physical) craving beyond mental control."[9]
In professional and research contexts, the term "alcoholism" sometimes encompasses both alcohol abuse and alcohol dependence, and sometimes is considered equivalent to alcohol dependence. Alcoholism follows a progressive course: if a person continues to drink, their condition will worsen. This will lead to harmful consequences in their life, physically, mentally, emotionally and socially.[11]
The emotional progression of the addict's response to alcohol can be charted in four phases. The first two are considered "normal" drinking and the last two are viewed as "typical" alcoholic drinking:
- Learning the mood swing. A person is introduced to alcohol (in some cultures this can happen at a relatively young age), and the person enjoys the happy feeling it produces. At this stage, there is no emotional cost.
- Seeking the mood swing. A person will drink to regain that feeling of euphoria experienced in phase 1; the drinking will increase as more intoxication is required to achieve the same effect. Again at this stage, there are no significant consequences.
- At the third stage there are physical and social consequences, such as hangovers, family problems, work problems, and so forth. A person will continue to drink excessively, disregarding the problems.
- The fourth stage can be detrimental, including risk for premature death. As a person now drinks to feel normal, they block out the feelings of overwhelming guilt, remorse, anxiety, and shame they experience when sober.[11]
Alternatively, focus on the physical deterioration that alcohol consumption causes has been described in three stages:
- Adaptive stage – The person will not experience any negative symptoms, and they believe they have the capacity for drinking alcohol without problems. Physiological changes are happening with the increase in tolerance, but this will not be noticeable to the drinker or others.
- Dependent stage – At this stage, symptoms build up gradually. Hangover symptoms from excessive drinking may be confused with withdrawal symptoms. Many addicts will maintain their drinking to avoid withdrawal sickness, drinking small amounts frequently. They will try to hide their drinking problem from others and will avoid gross intoxication.
- Deterioration stage – Various organs are damaged due to long-term drinking. Medical treatment in a rehabilitation center will be required; otherwise, the pathological changes will cause death.[12]
DSM and ICD
In the United States, the Diagnostic and Statistical Manual of Mental Disorders (DSM) which is generally used in psychology and psychiatry, is the most common diagnostic guide for substance use disorders, whereas most countries use the International Classification of Diseases (ICD), which is most used in medicine for physical problems, for diagnostic (and other) purposes. The two manuals use similar but not identical nomenclature to classify alcohol problems. Also, both guides have been updated in recent years. The table below shows the two most recent versions of each manual.
| Manual | Nomenclature | Definition |
|---|---|---|
| DSM-IV | Alcohol abuse, or Alcohol dependence |
|
| DSM-5 | Alcohol use disorder | "A problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by [two or more symptoms out of a total of 12], occurring within a 12-month period"[15] |
| ICD-10 | Alcohol harmful use, or Alcohol dependence syndrome | Definitions are similar to that of the DSM-IV. The World Health Organization uses the term "alcohol dependence syndrome" rather than alcoholism.<rhttps://apps.who.int/iris/handle/10665/39461 Lexicon of alcohol and drug terms] World Health Organization. Retrieved June 30, 2022.</ref> The concept of "harmful use" (as opposed to "abuse") was introduced in 1992's ICD-10 to minimize underreporting of damage in the absence of dependence. The term "alcoholism" was removed from ICD between ICD-8/ICDA-8 and ICD-9.[16] |
| ICD-11 | Episode of harmful use of alcohol, Harmful pattern of use of alcohol, or Alcohol dependence |
|
Urine and blood tests
There are reliable tests for the actual use of alcohol, one common test being that of blood alcohol content (BAC). These tests do not differentiate alcoholics from non-alcoholics. BAC is useful to judge alcohol tolerance, which in turn is a sign of alcoholism.[20] Long-term heavy drinking does have several recognizable effects on the body, including:
- Macrocytosis (enlarged MCV)
- Elevated GGT
- Moderate elevation of AST and ALT and an AST: ALT ratio of 2:1
- High carbohydrate deficient transferrin (CDT)
- Electrolyte and acid-base abnormalities including hypokalemia, hypomagnesemia, hyponatremia, hyperuricemia, metabolic acidosis, and respiratory alkalosis are common in alcoholics.[21]
However, none of these blood tests for biological markers is as sensitive as screening questionnaires.
Screening
Several tools may be used to detect a loss of control of alcohol use. These tools are mostly self-reports in questionnaire form.
The CAGE questionnaire, named for its four questions, is one such example that may be used to screen patients quickly in a doctor's office.[22]
Two "yes" responses indicate that the respondent should be investigated further.
The questionnaire asks the following questions:
- Have you ever felt you needed to Cut down on your drinking?
- Have people Annoyed you by criticizing your drinking?
- Have you ever felt Guilty about drinking?
- Have you ever felt you needed a drink first thing in the morning (Eye-opener) to steady your nerves or to get rid of a hangover?
- The CAGE questionnaire has demonstrated a high effectiveness in detecting alcohol-related problems; however, it has limitations in people with less severe alcohol-related problems.
Other tests are sometimes used for the detection of alcohol dependence, such as the Alcohol Dependence Data Questionnaire (SADD), which is a more sensitive diagnostic test than the CAGE questionnaire. It helps distinguish a diagnosis of alcohol dependence from one of heavy alcohol use.[23]
The Michigan Alcohol Screening Test (MAST) is a screening tool for alcoholism widely used by courts to determine the appropriate sentencing for people convicted of alcohol-related offenses,[24] driving under the influence being the most common.
The Alcohol Use Disorders Identification Test (AUDIT), a screening questionnaire developed by the World Health Organization, is unique in that it has been validated in six countries and is used internationally. Like the CAGE questionnaire, it uses a simple set of questions – a high score earning a deeper investigation.[25]
The Paddington Alcohol Test (PAT) was designed to screen for alcohol-related problems amongst those attending Accident and Emergency departments. It accords well with the AUDIT questionnaire but is administered in a fifth of the time.[26]
Signs and symptoms
The risk of alcohol dependence begins at low levels of drinking and increases directly with both the volume of alcohol consumed and a pattern of drinking larger amounts on an occasion, to the point of intoxication.
Women are generally more sensitive than men to the harmful effects of alcohol, primarily due to their smaller body weight, lower capacity to metabolize alcohol, and higher proportion of body fat.[27]
The recommended daily limits for moderate alcohol consumption are no more than 2 drinks for men or 1 drink for women per day. According to the National Institute on Alcohol Abuse and Alcoholism [NIAAA], men may be at risk for alcohol-related problems if their alcohol consumption exceeds 14 standard drinks per week or four drinks per day, and women may be at risk if they have more than 7 standard drinks per week or 3 drinks per day. A standard drink is defined as one 12-ounce bottle of beer, one 5-ounce glass of wine, or 1.5 ounces of distilled spirits. "Binge drinking" is defined as consuming 5 or more drinks (4 or more for women) in about 2 hours at least once in the past month. Drinking heavily is defined as consuming 5 or more drinks in one day or 15 in one week (4 or more in 1 day or 8 or more in a week for women).[28]
Long-term misuse
Alcoholism is characterized by an increased tolerance to alcohol – which means that an individual can consume more alcohol – and physical dependence on alcohol, which makes it hard for an individual to control their consumption. The physical dependency caused by alcohol can lead to an affected individual having a very strong urge to drink alcohol. These characteristics play a role in decreasing an alcoholic's ability to stop drinking.[29] Alcoholism can have adverse effects on mental health, contributing to psychiatric disorders and increasing the risk of suicide. A depressed mood is a common symptom of heavy alcohol drinkers.[30]
Warning signs
Warning signs of alcoholism include the consumption of increasing amounts of alcohol and frequent intoxication, preoccupation with drinking to the exclusion of other activities, promises to quit drinking and failure to keep those promises, the inability to remember what was said or done while drinking (colloquially known as "blackouts"), personality changes associated with drinking, denial or the making of excuses for drinking, the refusal to admit excessive drinking, dysfunction or other problems at work or school, the loss of interest in personal appearance or hygiene, marital and economic problems, and the complaint of poor health, with loss of appetite, respiratory infections, or increased anxiety.
Physical
Short-term effects
Drinking enough to cause a blood alcohol concentration (BAC) of 0.03–0.12 percent typically causes an overall improvement in mood and possible euphoria (a "happy" feeling), increased self-confidence and sociability, decreased anxiety, a flushed, red appearance in the face and impaired judgment and fine muscle coordination. A BAC of 0.09 percent to 0.25 percent causes lethargy, sedation, balance problems, and blurred vision. A BAC of 0.18 percent to 0.30 percent causes profound confusion, impaired speech (such as slurred speech), staggering, dizziness, and vomiting. A BAC from 0.25 percent to 0.40 percent causes stupor, unconsciousness, anterograde amnesia, vomiting (death may occur due to inhalation of vomit (pulmonary aspiration) while unconscious), and respiratory depression (potentially life-threatening). A BAC from 0.35 percent to 0.80 percent causes a coma (unconsciousness), life-threatening respiratory depression, and possibly fatal alcohol poisoning. With all alcoholic beverages, drinking while driving, operating an aircraft or heavy machinery increases the risk of an accident; many countries have penalties for drunk driving.
Long-term effects
Long-term alcohol use can affect all parts of the body, but it particularly affects the brain, heart, liver, pancreas, and immune system. Alcoholism can result in mental illness, delirium tremens, Wernicke–Korsakoff syndrome, irregular heartbeat, an impaired immune response, liver cirrhosis, and increased cancer risk.[20]
Having more than one drink a day for women or two drinks for men increases the risk of heart disease, high blood pressure, atrial fibrillation, and stroke. Risk is greater in younger people due to binge drinking, which may result in violence or accidents.[31]
Women develop long-term complications of alcohol dependence more rapidly than do men. Additionally, women have a higher mortality rate from alcoholism than men. Heavy drinking over time has been found to have a negative effect on reproductive functioning in women. This results in reproductive dysfunction such as anovulation, decreased ovarian mass, problems or irregularity of the menstrual cycle, and early menopause.[32]
Psychiatric
Long-term misuse of alcohol can cause a wide range of mental health problems. Severe cognitive problems are common; approximately 10 percent of all dementia cases are related to alcohol consumption, making it the second leading cause of dementia.[33] Psychiatric disorders are common in alcoholics, with the most prevalent psychiatric symptoms being anxiety and depression disorders.
Psychiatric disorders differ depending on gender. Women who have alcohol-use disorders often have a co-occurring psychiatric diagnosis such as major depression, anxiety, panic disorder, bulimia, post-traumatic stress disorder (PTSD), or borderline personality disorder. Men with alcohol-use disorders more often have a co-occurring diagnosis of narcissistic or antisocial personality disorder, bipolar disorder, schizophrenia, impulse disorders or attention deficit/hyperactivity disorder (ADHD). Women with alcoholism are more likely to experience physical or sexual assault, abuse and domestic violence than women in the general population,[34] which can lead to higher instances of psychiatric disorders and greater dependence on alcohol.
Social effects
Social skills are significantly impaired in people suffering from alcoholism due to the intoxicating effects of alcohol and the neurotoxic effects of alcohol on the brain, especially the prefrontal cortex area of the brain. The social skills that are impaired by alcohol abuse include impairments in perceiving facial emotions, prosody perception problems and theory of mind deficits; the ability to understand humor is also impaired in alcohol abusers.[35]
Alcohol abuse is associated with an increased risk of committing criminal offences, including child abuse, domestic violence, rape, burglary, and assault.[36] Alcoholism is associated with loss of employment, which can lead to financial problems. Drinking at inappropriate times and behavior caused by reduced judgment can lead to legal consequences, such as criminal charges for drunk driving[37] or public disorder, or civil penalties for tortious behavior, and may lead to a criminal sentence.
An alcoholic's behavior and mental impairment while drunk can profoundly affect those surrounding him and lead to isolation from family and friends. This isolation can lead to marital conflict and divorce, or contribute to domestic violence. Alcoholism can also lead to child neglect, with subsequent lasting damage to the emotional development of the alcoholic's children. For this reason, children of alcoholic parents can develop a number of emotional problems.
Alcohol withdrawal
As with similar substances with a sedative-hypnotic mechanism, such as barbiturates and benzodiazepines, withdrawal from alcohol dependence can be fatal if it is not properly managed.[38][39] Alcohol's primary effect is the increase in stimulation of the GABAA receptor, promoting central nervous system depression. With repeated heavy consumption of alcohol, these receptors are desensitized and reduced in number, resulting in tolerance and physical dependence. When alcohol consumption is stopped too abruptly, the person's nervous system suffers from uncontrolled synapse firing. This can result in symptoms that include anxiety, life-threatening seizures, delirium tremens, hallucinations, shakes, and possible heart failure.[40]
The acute withdrawal phase can be defined as lasting between one and three weeks. Severe acute withdrawal symptoms such as delirium tremens and seizures rarely occur after one-week post cessation of alcohol. In the period of three–six weeks following cessation increased anxiety, depression, as well as sleep disturbance, is common;[41] fatigue and tension can persist for up to 5 weeks as part of the post-acute withdrawal syndrome; about a quarter of alcoholics experience anxiety and depression for up to two years.
A kindling effect also occurs in alcoholics whereby each subsequent withdrawal syndrome is more severe than the previous withdrawal episode; this is due to neuroadaptations which occur as a result of periods of abstinence followed by re-exposure to alcohol. Individuals who have had multiple withdrawal episodes are more likely to develop seizures and experience more severe anxiety during withdrawal from alcohol than alcohol-dependent individuals without a history of past alcohol withdrawal episodes. The kindling effect leads to persistent functional changes in brain neural circuits as well as to gene expression.[42] Kindling also results in the intensification of psychological symptoms of alcohol withdrawal.
Treatment
Attitudes and social stereotypes can create barriers to the detection and treatment of alcohol abuse. This is more of a barrier for women than men. Fear of stigmatization may lead women to deny that they are suffering from a medical condition, to hide their drinking, and to drink alone. This pattern, in turn, leads family and others to be less likely to suspect that a woman they know is an alcoholic.[32] In contrast, reduced fear of stigma may lead men to admit that they are suffering from a medical condition, to display their drinking publicly, and to drink in groups.
The treatment community for alcoholism typically supports an abstinence-based zero tolerance approach which focuses on helping people discontinue their alcohol intake, followed up with life training and/or social support to help them resist a return to alcohol use. Since alcoholism involves multiple factors which encourage a person to continue drinking, they must all be addressed to successfully prevent a relapse. An example of this kind of treatment is detoxification followed by a combination of supportive therapy, attendance at self-help groups, and ongoing development of coping mechanisms. However, some prefer a harm-reduction approach.[43]
Detoxification
Alcohol detoxification or 'detox' for alcoholics is an abrupt stop of alcohol drinking coupled with the substitution of drugs, such as benzodiazepines, that have similar effects to prevent alcohol withdrawal. Individuals who are only at risk of mild to moderate withdrawal symptoms can be detoxified as outpatients. Individuals at risk of a severe withdrawal syndrome as well as those who have significant or acute comorbid conditions are generally treated as inpatients. Detoxification does not actually treat alcoholism, and it is necessary to follow up detoxification with an appropriate treatment program for alcohol dependence or abuse to reduce the risk of relapse. Some symptoms of alcohol withdrawal, such as depressed mood and anxiety, typically take weeks or months to abate while other symptoms persist longer due to persisting neuroadaptations.
Psychological
Various forms of group therapy or psychotherapy can be used to deal with underlying psychological issues that are related to alcohol addiction, as well as provide relapse prevention skills. The mutual-help group-counseling approach is one of the most common ways of helping alcoholics maintain sobriety. Alcoholics Anonymous was one of the first organizations formed to provide mutual, nonprofessional counseling, and it is still the largest. Alcoholics Anonymous and twelve-step programs appear more effective than cognitive behavioral therapy or abstinence.[44]
Moderate drinking
Rationing and moderation programs such as Moderation Management and DrinkWise do not mandate complete abstinence. While most alcoholics are unable to limit their drinking in this way, some return to moderate drinking.
A 2002 US study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) showed that 17.7 percent of individuals diagnosed as alcohol dependent more than one year prior returned to low-risk drinking. This group, however, showed fewer initial symptoms of dependency.[45] A follow-up study, using the same subjects that were judged to be in remission in 2001–2002, examined the rates of return to problem drinking in 2004–2005. The study found abstinence from alcohol was the most stable form of remission for recovering alcoholics.[46]
Medications
In the United States there are three approved medications for alcoholism: acamprosate, naltrexone, and disulfiram.[47]
- Acamprosate may stabilize the brain chemistry that is altered due to alcohol dependence via antagonizing the actions of glutamate, a neurotransmitter which is hyperactive in the post-withdrawal phase. By reducing excessive NMDA activity which occurs at the onset of alcohol withdrawal, acamprosate can reduce or prevent alcohol withdrawal related neurotoxicity. Research with this medication has produced mixed result, with the most success in patients who develop alcohol dependence later in life and who display physical dependence and higher than usual levels of anxiety.[47]
- Disulfiram prevents the elimination of acetaldehyde, a chemical the body produces when breaking down ethanol. Acetaldehyde itself is the cause of many hangover symptoms from alcohol use. The overall effect is discomfort when alcohol is ingested, including reddening or flushing of the face and neck, nausea, and nervousness.[47]
- Naltrexone is a competitive antagonist for opioid receptors, effectively blocking the effects of endorphins and opioids which lead to addiction. Alcohol causes the body to release endorphins, which in turn release dopamine and activate the reward pathways; hence in the body reduces the pleasurable effects from consuming alcohol. Naltrexone is used to decrease cravings for alcohol and encourage abstinence. Evidence supports a reduced risk of relapse among alcohol-dependent persons and a decrease in excessive drinking.[47]
- The Sinclair method is another approach to using naltrexone or other opioid antagonists to treat alcoholism by having the person take the medication about an hour before they drink alcohol and only then. The medication blocks the positive reinforcement effects of ethanol and hypothetically allows the person to stop drinking or drink less. This method uses the nervous system’s own mechanism to gradually remove interest in alcohol and the behaviors involved in alcohol drinking.[48]
Several other drugs are also used and many are under investigation, including
- Benzodiazepines, while useful in the management of acute alcohol withdrawal, if used long-term can cause a worse outcome in alcoholism. Alcoholics on chronic benzodiazepines have a lower rate of achieving abstinence from alcohol than those not taking benzodiazepines. This class of drugs is commonly prescribed to alcoholics for insomnia or anxiety management.[49]
- Calcium carbimide works in the same way as disulfiram; it has an advantage in that the occasional adverse effects of disulfiram, hepatotoxicity and drowsiness, do not occur with calcium carbimide.[50]
Prognosis
Alcoholism may reduce a person's life expectancy by several years. The most common cause of death in alcoholics is from cardiovascular complications.[51] There is a high rate of suicide in chronic alcoholics, which increases the longer a person drinks.[52]
There is a substantial level of recovery from alcohol dependence, although those who can be classified as in recovery still constitute less than 50 percent of alcoholics. A major study found that of the group of people classified with DSM–IV alcohol dependence, 25.0 percent were still classified as dependent in the past year; 27.3 percent were classified as being in partial remission; 11.8 percent were asymptomatic risk drinkers who demonstrated a pattern of drinking that put them at risk of relapse; 17.7 percent were low-risk drinkers, classified as being in nonabstinent recovery (NR); and 18.2 percent were abstainers, classified as in abstinent recovery (AR). Only 25.5 percent of the people in the study had received treatment.[45]
Causes
A complex mixture of genetic and environmental factors influences the risk of the development of alcoholism.[53] Someone with a parent or sibling with alcoholism is three to four times more likely to become an alcoholic themselves. High stress levels and anxiety, as well as alcohol's inexpensive cost and easy accessibility, increase the risk.[20] Severe childhood trauma and lack of peer and family support are also associated with an increased risk of alcoholism developing.[53]
Availability
Alcohol is the most available, widely consumed, and widely abused recreational drug. Beer alone is the world's most widely consumed alcoholic beverage; it is the third-most popular drink overall, after water and tea.[54] It is thought to be the oldest fermented beverage.[55]
Genetic variation
There are genetic variations that affect the risk for alcoholism.[56][53] The variants with strongest effect are in genes that encode the main enzymes of alcohol metabolism, ADH1B and ALDH2. These genetic factors influence the rate at which alcohol and its initial metabolic product, acetaldehyde, are metabolized.[56] They are found at different frequencies in people from different parts of the world. The alcohol dehydrogenase allele ADH1B*2 causes a more rapid metabolism of alcohol to acetaldehyde, and reduces risk for alcoholism; it is most common in individuals from East Asia and the Middle East. The alcohol dehydrogenase allele ADH1B*3 causes a more rapid metabolism of alcohol, leading to a reduced risk of developing alcoholism. The allele ADH1B*3 is only found in some individuals of African descent and certain Native American tribes. The aldehyde dehydrogenase allele ALDH2*2 greatly reduces the rate at which acetaldehyde, the initial product of alcohol metabolism, is removed by conversion to acetate; it greatly reduces the risk for alcoholism.[56]
Individuals who have a genetic disposition to alcoholism are also more likely to begin drinking at an earlier age than average, and a younger age of onset of drinking is associated with an increased risk to develop alcohol-related problems.[57] However, it is not entirely clear whether this association is causal.
Prevention
The World Health Organization, the European Union, and other regional bodies, national governments and parliaments have formed alcohol policies in order to reduce the harm of alcoholism. These include regulating and limiting the sale of alcohol particularly to younger people, taxing alcohol to increase its cost, and providing inexpensive treatment.[58]
Targeting adolescents and young adults is regarded as an important step to reduce the harm of alcohol abuse. Increasing the age at which licit drugs of abuse such as alcohol can be purchased, the banning or restricting advertising of alcohol has been recommended as additional ways of reducing the harm of alcohol dependence and abuse. Credible, evidence based educational campaigns in the mass media about the consequences of alcohol abuse have been recommended. Guidelines for parents to prevent alcohol abuse amongst adolescents, and for helping young people with mental health problems have also been suggested.[59]
Epidemiology
Substance use disorders are a major public health problem facing many countries, and "the most common substance of abuse/dependence in patients presenting for treatment is alcohol."[43]
The World Health Organization has reported that three million deaths every year result from harmful use of alcohol, that harmful use of alcohol is a causal factor in more than 200 disease and injury conditions, and that overall 5.1 percent of the global burden of disease and injury is attributable to alcohol.[58]
Within the medical and scientific communities, there is a broad consensus regarding alcoholism as a disease state. Alcoholism is most common among males and young adults, and is less common in middle and old age.[20] In recent decades, however, the proportion of female alcoholics has increased. Most alcoholics develop alcoholism during adolescence or young adulthood.[53] 31 percent of college students show signs of alcohol abuse, while six percent are dependent on alcohol. Under the DSM's definition of alcoholics, that means about 37 percent of college students could meet the criteria.[60]
Society and culture
The various health problems associated with long-term alcohol consumption are generally perceived as detrimental to society. For example, money due to lost labor-hours, medical costs due to injuries from to drunkenness, and organ damage from long-term use, and secondary treatment costs, such as the costs of rehabilitation facilities and detoxification centers.
Beyond the financial costs that alcohol consumption imposes, there are also significant social costs to both the alcoholic and their family and friends.[38] For instance, alcohol consumption by a pregnant woman can lead to an incurable and damaging condition known as fetal alcohol syndrome, which often results in cognitive deficits, mental health problems, an inability to live independently and an increased risk of criminal behavior, all of which can cause emotional stress for parents and caregivers.[61]
Many terms, some insulting and others informal, have been used to refer to people affected by alcoholism. Such expressions include "tippler," "drunkard," "dipsomaniac," and "souse."[62] Stereotypes of alcoholics are often found in fiction and popular culture. The "town drunk" is a stock character in Western popular culture. Stereotypes of drunkenness may be based on xenophobia, as in the fictional depiction of the Irish as heavy drinkers.[63]
Notes
- ↑ R.M. Morse and D.K. Flavin, The definition of alcoholism. The Joint Committee of the National Council on Alcoholism and Drug Dependence and the American Society of Addiction Medicine to Study the Definition and Criteria for the Diagnosis of Alcoholism JAMA 268(8) (1992): 1012–1014. Retrieved December 28, 2023.
- ↑ Uwe Henrik Peters, Lexikon Psychiatrie, Psychotherapie, Medizinische Psychologie (Urban & Fischer/Elsevier, 2016, ISBN 978-3437150630).
- ↑ Mariana Valverde, Diseases of the Will (Cambridge University Press, 1998, ISBN 978-0521623001).
- ↑ Sarah W. Tracy, Alcoholism in America: From Reconstruction to Prohibition (Johns Hopkins University Press, 2005, ISBN 978-0801881190).
- ↑ Magnus Huss, Alcoholismus Chronicus (Forgotten Books, 2018, ISBN 978-0428121662).
- ↑ J.S. Blocker, Did Prohibition Really Work? Alcohol Prohibition as a Public Health Innovation American Journal of Public Health 96(2) (2006): 233-243. Retrieved December 28, 2023.
- ↑ Jill Littrell, Understanding and Treating Alcoholism Volume I: An Empirically Based Clinician's Handbook for the Treatment of Alcoholism (Psychology Press, 1991, ISBN 978-0805808704).
- ↑ Deborah Hasin, Classification of Alcohol Use Disorders National Institute on Alcohol Abuse and Alcoholism, December 2003. Retrieved December 28, 2023.
- ↑ 9.0 9.1 Alcoholics Anonymous, Alcoholics Anonymous (The Big Book) (Alcoholics Anonymous World Services, 2001, ISBN 978-1893007161).
- ↑ Thomas F. McGovern and William L. White, Alcohol Problems in the United States: Twenty Years of Treatment Perspective (Routledge, 2003, ISBN 978-0789020482).
- ↑ 11.0 11.1 Dennis L. Thombs and Cynthia J. Osborn, Introduction To Addictive Behaviors (The Guilford Press, 2019, ISBN 978-1462539222).
- ↑ Amy Keller, Stages of Alcoholism Drug Rehab, February 28, 2020. Retrieved December 28, 2023.
- ↑ 13.0 13.1 Gary R. VandenBos (ed.), APA Dictionary of Psychology (American Psychological Association, 2015, ISBN 978-1433819445).
- ↑ Christopher S. Martin and Tammy Chung, How Should We Revise Diagnostic Criteria for Substance Use Disorders in the DSM—V? J. Abnorm Psychol. 117(3) (August 2008): 561–575. Retrieved December 28, 2023.
- ↑ American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (American Psychiatric Publishing, 2013, ISBN 978-0890425541).
- ↑ A System to Convert ICD Diagnostic Codes for Alcohol Research Morbidity and Mortality Weekly Report, August 5, 1998. Retrieved December 28, 2023.
- ↑ Episode of harmful use of alcohol ICD-11 for Mortality and Morbidity Statistics, April, 2019. Retrieved December 28, 2023.
- ↑ Harmful pattern of use of alcohol ICD-11 for Mortality and Morbidity Statistics, April, 2019. Retrieved December 28, 2023.
- ↑ 6C40.2 Alcohol dependence ICD-11 for Mortality and Morbidity Statistics, April, 2019. Retrieved December 28, 2023.
- ↑ 20.0 20.1 20.2 20.3 American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (American Psychiatric Publishing, 2013, ISBN 978-0890425558).
- ↑ Alcohol's Effects on the Body National Institute on Alcohol Abuse and Alcoholism (NIAAA). Retrieved December 28, 2023.
- ↑ What is the CAGE questionnaire? Healthline. Retrieved December 28, 2023.
- ↑ Alcohol Dependence Data Questionnaire (SADD) European Monitoring Centre for Drugs and Drug Addiction, July 15, 2004. Retrieved December 28, 2023.
- ↑ The Michigan Alcohol Screening Test American Addiction Centers, November 30, 2023. Retrieved December 28, 2023.
- ↑ AUDIT : the Alcohol Use Disorders Identification Test : guidelines for use in primary health care World Health Organization, November 18, 2001. Retrieved December 28, 2023.
- ↑ S.G. Smith, R. Touquet, S. Wright, and N. Das Gupta, Detection of alcohol misusing patients in accident and emergency departments: the Paddington alcohol test (PAT) J Accid Emerg Med. 13(5) (September 1996): 308–312. Retrieved December 28, 2023.
- ↑ World Health Organization, Global Status Report on Alcohol and Health 2018 (World Health Organization, 2019, ISBN 978-9241565639).
- ↑ Drinking Levels Defined National Institute on Alcohol Abuse and Alcoholism (NIAAA). Retrieved December 28, 2023.
- ↑ P.L. Hoffman and B. Tabakoff, Alcohol dependence: a commentary on mechanisms Alcohol and Alcoholism 31(4) (July 1996): 333–340. Retrieved December 28, 2023.
- ↑ Richard Wilson and Cheryl Kolander, Drug Abuse Prevention: A School and Community Partnership (Jones & Bartlett Learning, 2010, ISBN 978-0763771584).
- ↑ James H. O’Keefe, Salman K. Bhatti, Ata Bajwa, James J. DiNicolantonio, and Carl J. Lavie, Alcohol and Cardiovascular Health: The Dose Makes the Poison…or the RemedyMayo Clinic Proceedings 89(3) (March 1, 2014): 382-393. Retrieved December 28, 2023.
- ↑ 32.0 32.1 L.N. Blum, N.H. Nielsen, and J.A. Riggs, Alcoholism and alcohol abuse among women: report of the Council on Scientific Affairs J Womens Health 7(7) (September 1998): 861-871. Retrieved December 28, 2023.
- ↑ Georgy Bakalkin, Alcoholism-associated molecular adaptations in brain neurocognitive circuits European College of Neuropsychopharmacology, July 8, 2008. Retrieved December 28, 2023.
- ↑ Brad R. Karoll, Women and Alcohol-Use Disorders: A Review of Important Knowledge and Its Implications for Social Work Practitioners Journal of Social Work, December 1, 2002. Retrieved December 28, 2023.
- ↑ Jennifer Uekermann and Irene Daum, Social cognition in alcoholism: a link to prefrontal cortex dysfunction? Addiction 103(5) (May 2008): 726–735. Retrieved December 28, 2023.
- ↑ Richard Isralowitz, Drug Use: A Reference Handbook (ABC-CLIO, 2004, ISBN 978-1576077085).
- ↑ Maria Gifford, Alcoholism (Biographies of Disease) (Greenwood, 2009, ISBN 978-0313359088).
- ↑ 38.0 38.1 Chris McCully, Goodbye, Mr. Wonderful: Alcoholism, Addiction and Early Recovery (Jessica Kingsley, 2004, ISBN 978-1843102656).
- ↑ Marc Galanter, Herbert D. Kleber, and Kathleen T. Brady (eds.), The American Psychiatric Publishing Textbook of Substance Abuse Treatment (American Psychiatric Publishing, 2014, ISBN 978-1585624720).
- ↑ Richard C. Dart, Medical Toxicology (Lippincott Williams & Wilkins, 2003, ISBN 978-0781728454).
- ↑ Markus Heilig, Mark Egli, John C. Crabbe, and Howard C. Becker, Acute withdrawal, protracted abstinence and negative affect in alcoholism: are they linked? Addict Biol 15(2) (April 2010): 169-184. Retrieved December 28, 2023.
- ↑ George R. Breese, Rajita Sinha, and Markus Heilig, Chronic alcohol neuroadaptation and stress contribute to susceptibility for alcohol craving and relapse Pharmacol Ther 129(2) (February 2011): 149–171. Retrieved December 28, 2023.
- ↑ 43.0 43.1 Glen O. Gabbard, Treatments of psychiatric disorders (American Psychiatric Publications, 2014, ISBN 978-1585624423).
- ↑ John F. Kelly, Keith Humphreys, and Marica Ferri, Alcoholics Anonymous and other 12‐step programs for alcohol use disorder Cochrane Database of Systematic Reviews, March 11, 2020. Retrieved December 28, 2023.
- ↑ 45.0 45.1 Deborah A. Dawson, Bridget F. Grant, Frederick S. Stinson, Patricia S. Chou, Boji Huang, and W. June Ruan, Recovery From DSM–IV Alcohol Dependence Addiction 100(3) (2005):281–292. Retrieved December 28, 2023.
- ↑ Deborah A. Dawson, Risë B. Goldstein, and Bridget F. Grant, Rates and Correlates of Relapse Among Individuals in Remission From DSM-IV Alcohol Dependence: A 3-Year Follow-Up Alcoholism Clinical & Experimental Research 31(12) (December 2007): 2036-2045. Retrieved December 28, 2023.
- ↑ 47.0 47.1 47.2 47.3 Barbara J. Mason, What Medications Are Used to Treat Alcohol Use Disorder? National Institute on Alcohol Abuse and Alcoholism (NIAAA). Retrieved December 28, 2023.
- ↑ What is the Sinclair Method? Sinclair Method. Retrieved December 28, 2023.
- ↑ Stan Lindsay and Graham E. Powell (eds.), The Handbook of Clinical Adult Psychology (Routledge, 2007, ISBN 978-1583918661).
- ↑ A.C. Ogborne, Identifying and treating patients with alcohol-related problems CMAJ 162(12) (June 13 2000): 1705–1708. Retrieved December 28, 2023.
- ↑ Eugenija Zuskin et al., Alcoholism—how it affects health and working capacity Archives of Industrial Hygiene and Toxicology 57(4) (2007):413-426. Retrieved December 28, 2023.
- ↑ American Psychiatric Association, American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders (American Psychiatric Publishing, 2006, ISBN 978-0890423851).
- ↑ 53.0 53.1 53.2 53.3 Mary-Anne Enoch, Genetic and environmental influences on the development of alcoholism: resilience vs. risk Annals of the New York Academy of Sciences 1094 (2006): 193–201. Retrieved December 28, 2023.
- ↑ Max Nelson, The Barbarian's Beverage: A History of Beer in Ancient Europe (Routledge, 2005, ISBN 978-0415311212).
- ↑ Richard Rudgley, The Alchemy of Culture: Intoxicants in Society (British Museum Press, 1993, ISBN 978-0714117362).
- ↑ 56.0 56.1 56.2 Howard J. Edenberg and Jeanette N. McClintick, Alcohol Dehydrogenases, Aldehyde Dehydrogenases, and Alcohol Use Disorders: A Critical Review Alcoholism: Clinical and Experimental Research 42(12) (2018):2281–2297. Retrieved December 28, 2023.
- ↑ Arpana Agrawal and Carol A. Prescott, Early Age At First Drink May Modify Tween/Teen Risk For Alcohol Dependence Alcoholism: Clinical & Experimental Research (September 2009). Retrieved December 28, 2023.
- ↑ 58.0 58.1 Alcohol World Health Organization, May 9, 2022. Retrieved December 28, 2023.
- ↑ Fulton Crews, Jun He, and Clyde Hodge, Adolescent cortical development: a critical period of vulnerability for addiction Pharmacol Biochem Behav 86(2) (February 2007): 189–199. Retrieved December 28, 2023.
- ↑ Megan Sanderson, About 37 percent of college students could now be considered alcoholics Daily Emerald (November 5, 2018). Retrieved December 28, 2023.
- ↑ Ann Streissguth, Fetal Alcohol Syndrome: A Guide for Families and Communities (Brookes Publishing, 1997, ISBN 978-1557662835).
- ↑ Chambers, The Chambers Thesaurus (Chambers, 2015, ISBN 978-1473608283).
- ↑ Richard Stivers, Hair of the Dog: Irish Drinking and its American Stereotype (Resource Publications (CA), 2019, ISBN 978-1532689871).
ReferencesISBN links support NWE through referral fees
- Alcoholics Anonymous. Alcoholics Anonymous (The Big Book). Alcoholics Anonymous World Services, 2001. ISBN 978-1893007161
- American Psychiatric Association. American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders. American Psychiatric Publishing, 2006. ISBN 978-0890423851
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. American Psychiatric Publishing, 2013. ISBN 978-0890425541
- Chambers. The Chambers Thesaurus. Chambers, 2015. ISBN 978-1473608283
- Dart, Richard C. Medical Toxicology. Lippincott Williams & Wilkins, 2003. ISBN 978-0781728454
- Gabbard, Glen O. Treatments of Psychiatric Disorders. American Psychiatric Publications, 2014. ISBN 978-1585624423
- Galanter, Marc, Herbert D. Kleber, and Kathleen T. Brady (eds.). The American Psychiatric Publishing Textbook of Substance Abuse Treatment. American Psychiatric Publishing, 2014. ISBN 978-1585624720
- Gifford, Maria. Alcoholism (Biographies of Disease). Greenwood, 2009. ISBN 978-0313359088
- Huss, Magnus. Alcoholismus Chronicus. Forgotten Books, 2018. ISBN 978-0428121662
- Isralowitz, Richard. Drug Use: A Reference Handbook. ABC-CLIO, 2004. ISBN 978-1576077085
- Lindsay, Stan, and Graham E. Powell (eds.). The Handbook of Clinical Adult Psychology. Routledge, 2007. ISBN 978-1583918661
- Littrell, Jill. Understanding and Treating Alcoholism Volume I: An Empirically Based Clinician's Handbook for the Treatment of Alcoholism. Psychology Press, 1991. ISBN 978-0805808704
- McCully, Chris. Goodbye, Mr. Wonderful: Alcoholism, Addiction and Early Recovery. Jessica Kingsley, 2004. ISBN 978-1843102656
- McGovern, Thomas F., and William L. White. Alcohol Problems in the United States: Twenty Years of Treatment Perspective. Routledge, 2003. ISBN 978-0789020482
- Nelson, Max. The Barbarian's Beverage: A History of Beer in Ancient Europe. Routledge, 2005. ISBN 978-0415311212
- Peters, Uwe Henrik. Lexikon Psychiatrie, Psychotherapie, Medizinische Psychologie. Urban & Fischer/Elsevier, 2016. ISBN 978-3437150630
- Rudgley, Richard. The Alchemy of Culture: Intoxicants in Society. British Museum Press, 1993. ISBN 978-0714117362
- Stivers, Richard. Hair of the Dog: Irish Drinking and its American Stereotype. Resource Publications (CA), 2019. ISBN 978-1532689871
- Streissguth, Ann. Fetal Alcohol Syndrome: A Guide for Families and Communities. Brookes Publishing, 1997. ISBN 978-1557662835
- Thombs, Dennis L., and Cynthia J. Osborn. Introduction To Addictive Behaviors. The Guilford Press, 2019. ISBN 978-1462539222
- Tracy, Sarah W. Alcoholism in America: From Reconstruction to Prohibition Johns Hopkins University Press, 2005. ISBN 978-0801881190
- Valverde, Mariana. Diseases of the Will. Cambridge University Press, 1998. ISBN 978-0521623001
- VandenBos, Gary R. (ed.). APA Dictionary of Psychology. American Psychological Association, 2015. ISBN 978-1433819445
- Wilson, Richard, and Cheryl Kolander. Drug Abuse Prevention: A School and Community Partnership. Jones & Bartlett Learning, 2010. ISBN 978-0763771584
- World Health Organization. Global Status Report on Alcohol and Health 2018. World Health Organization, 2019. ISBN 978-9241565639
External links
All links retrieved December 28, 2023.
- Alcohol use disorder Mayo Clinic
- Alcohol Use Disorder (AUD) Medline Plus
- Alcoholism American Addiction Centers
- Alcoholism and Alcohol Abuse Help Guide
- Alcoholism HealthLine
- Am I an Alcoholic? Villa Oasis
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.



